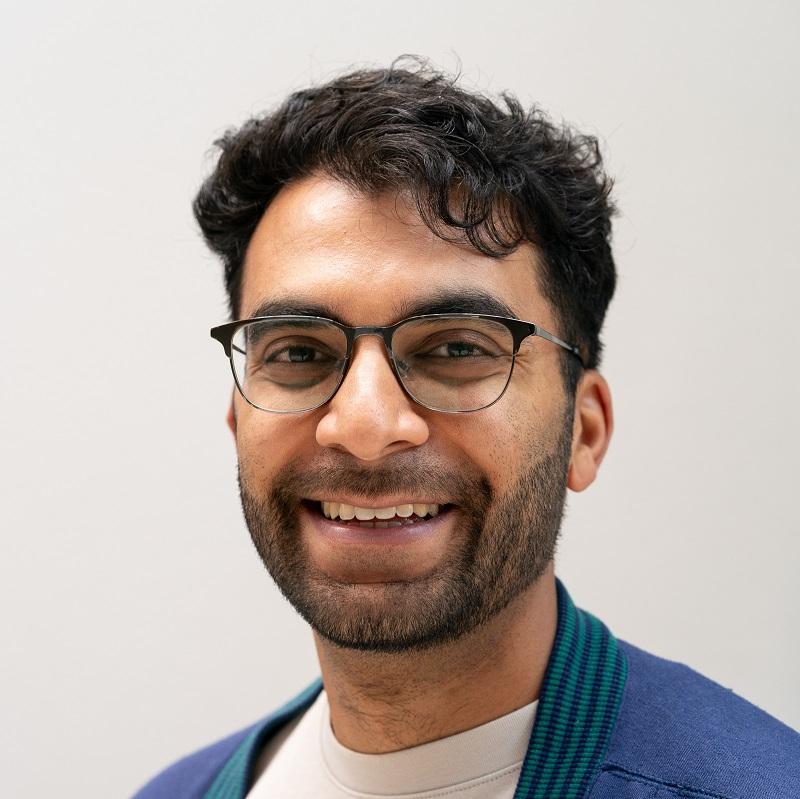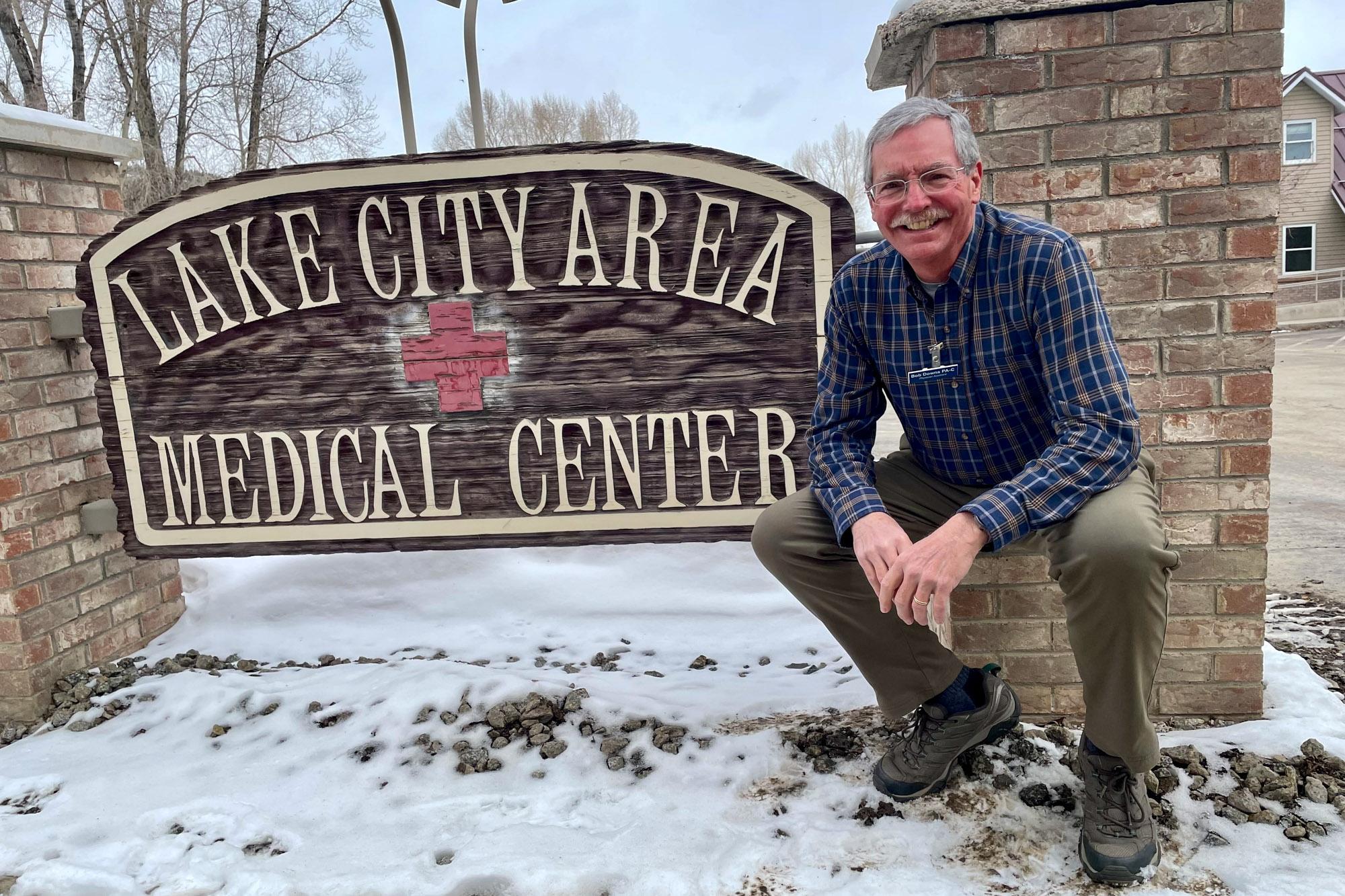
Bob Downs, 64, found his dream job through a small-town newspaper.
Downs, a physician assistant, was living in Dayton, Ohio, in 2014. The paper had been delivered from Lake City, CO, some 1,400 miles away. He and his wife had been subscribing for years after visiting the mountainous southwestern town.
The job posting — actually, it was a letter to the editor — said that the town’s medical clinic needed to replace a departing staff member.
“My wife and I looked at each other and said, you know, should I go for this?” Downs said. “I ended up getting the job. … I think on 60 days’ notice I was moving out here to fill the position.”
They moved to a county with a population of less than 800, and Downs joined a beleaguered but vital workforce: the rural medical corps. Small, rural clinics have increasingly come to rely on physician assistants like him, who can do much of the same work as doctors — with lower salaries and less medical schooling.
“I wanted to give something back for the last 10 or 12 years of my career, working in a smaller place where I really knew my patient population,” he said. Today, Downs is one of a handful of medical staffers at Lake City Area Medical Center, where one physician oversees a half-dozen nurses and assistants. It’s the largest medical facility for nearly 60 miles around.
Now, state lawmakers are working on a controversial proposal to expand and empower the ranks of physician assistants in rural clinics and elsewhere. A bill before the state legislature would allow experienced PAs — like Bob Downs — to work more independently of physicians, in hopes that it would attract more of them to rural settings and safety-net clinics.
“It’s a modest bill, but it’s very important to rural Colorado. It’ll increase access to care by updating existing restrictive laws and regulations,” said Republican state Rep. Perry Will. He’s co-sponsoring the measure with state Sen. Cleave Simpson, a Republican, and with state Rep. Susan Lontine and state Sen. Faith Winter, both Democrats.
“In rural areas, it’s hard to find physicians to supervise PAs,” Will continued. “This bill will allow experienced PAs to practice where they’re needed — within their scope, and while still consulting with … other members of the health care team as appropriate.”
The idea has led to unusual political divisions
Democratic lawmakers have argued fiercely among themselves on the House floor. Republicans also have split: Some agree with Will that the move will help with rural health shortages, while others argue that it will lead to substandard care.
“What is being presented as a solution is to say, ‘We’ll just lower the requirements for training, and hopefully fill the shortage in that way,’” said state Rep. Yadira Caraveo, a Democrat who is a physician and opposes the bill.
To become a PA requires completing a roughly three-year master’s degree-level program and logging thousands of hours of medical work experience. Under current law, physician assistants are closely tied to physicians. Even the most experienced PAs must have a doctor co-sign some of their work with patients.
Their scope of practice — what they can and can’t do — is based on the scope of their supervising physician. And PAs cannot practice at all if their clinic doesn’t have a doctor on staff, said Cooper Couch, the vice president of the Colorado Academy of Physician Assistants.

“Right now, if I have 10 years of experience and my physician retires, I cannot practice medicine until they hire a new physician,” said Couch, a PA who moved to Cañon City to work in a rural clinic.
The bill would remove legal language that says PAs must be supervised by doctors.
Instead, new PAs would make a “collaborative plan” with a physician — joining only a handful of states that allow PAs to work outside of direct supervision. And under the Colorado bill, those with more than 5,000 hours of experience would have even more independence.
It’s the rare bill that draws sharp debate among party members on both sides of the aisle. The opposition has been led by Caraveo, who is a pediatrician, and by state Rep. Kyle Mullica, a Democrat who works as a nurse.
“We both agree that this is not what’s best for our patients. We’re bringing a butcher knife to a problem that we need a scalpel for,” said Mullica, the majority co-whip.
During the debate, lawmakers argued sharply about the needs of rural Colorado.
State Rep. Lindsey Daugherty, a Democrat, said it would “literally put people’s lives at risk.”
State Rep. Matt Soper, a Republican in rural Delta County, said that the bill is part of the “war on rural Colorado,” because it implies that rural areas should accept care from PAs with less formal training.
In contrast, Republican state Rep. Patrick Neville said that the bill is a way to bridge “the rural-urban divide.” Giving more leeway to PAs would attract them to Colorado and fill out the rural workforce, he said.
“If they don’t have the ability to do that, they will absolutely flee the state,” he said.
Federally qualified health centers, often known as safety-net providers, often rely heavily on PAs.
For example, Sunrise Community Health employs about 52 practitioners in Northern Colorado. Only 12 are physicians, and most of the rest are PAs. It’s wasteful, said chief clinical officer Dr. Mark Wallace, to require those physicians to spend hours looking over the work of dozens of experienced PAs.
“To have my physicians continuously … do that level of supervision, it's not a value add, it's not enhancing the quality,” Wallace said in an interview. “Being able to remove that, I can now have my physicians spend their time in a much more collaborative model. They're actually freed up of oversight and paperwork.”
The bill has become something of a turf war between the different medical professions.
It’s opposed by several organizations representing physicians, including the Colorado Medical Society, according to state lobbying records.
Caraveo, the pediatrician lawmaker, worries that the change would lead people to attend PA school to get a cheaper, faster education.
“I believe that we need to be looking at incentivizing people to go through medical training, to train and practice at the top of their ability, and not changing the rules years after they’ve been established because we’re going through a moment of difficulty,” Caraveo said.
Advocates argue that PAs are not interested in supplanting doctors. They say that physician assistants would still use a team-based approach to health care, relying on other experts when they need help. They also argue that the state already allows many nurse practitioners, another type of medical professional, to perform similar clinical work without a physician’s supervision.
After a contentious earlier debate, the bill is set for its final votes in the House this week. Its fate, should it move on to the Senate, is uncertain. An earlier version was killed by Democrats in committee last year.