On April 6, Wendy Dikes got an upsetting email from her mother that said that her roommate at the Mesa Vista nursing home in Boulder was getting sick.
“My roommate coughs, and hacks like she is about to throw up,” Brenda Dikes, 69, said in the email.
Brenda figured that her roommate’s smoking caused the cough, but noted that nurses had left the roommate a mask to wear whenever she left the room.
As the week went on, Brenda started to believe that her roommate had COVID-19, the respiratory disease caused by the novel coronavirus. In follow-up emails to her daughter, Brenda said the nurses were checking in more often.
After a few days, staff closed the door to their room and told them they were both quarantined.
The new nurses who came in wore full protective suits.
Brenda has lived at Mesa Vista since 2017, where she receives around-the-clock care for multiple sclerosis and a heart condition. Like most others at nursing homes, Brenda’s pre-existing conditions and age make her vulnerable to developing a serious, and possibly deadly, case of COVID-19 if she contracts it.
Though Brenda has shown no symptoms, Wendy worries that she is at risk as long as she is quarantined with her roommate.
“We’re in a situation where I feel like my mom is basically condemned to die,” Wendy said. “Maybe that sounds a little dramatic but that is really how it feels."
The Dikes are just one of thousands of families across Colorado with a member in a long-term elder-care facility with cases of COVID-19. As of Tuesday, at least 78 elder-care facilities had outbreaks of COVID-19, which is defined by the state as having people in the facility with respiratory symptoms within a two-week period and at least one lab-confirmed case of COVID-19.
As of last week, deaths at nursing homes accounted for about one-third of the state’s total deaths from COVID-19.
Frustrated family members and elder-care residents have reported difficulties getting tests for suspected COVID-19 cases or finding updated information about the outbreak. Some, like Wendy Dikes, believe facilities are mishandling outbreaks.
Meanwhile, nursing homes report being overwhelmed by the disease, dealing with staffing shortages and an influx in calls from panicked family members.
Spokespeople from Vivage Senior Living, the company that owns Mesa Vista, and several dozen other nursing homes across the state, could not legally discuss specific patients at their facilities.
Speaking generally, Vivage officials said that state and federal guidance requires them to quarantine residents that have been exposed and that moving exposed residents could further spread the disease. They confirmed that, as of today, Mesa Vista has two positive cases of COVID-19.
“We are trying to provide information, but staff is overwhelmed right now,” Vivage CEO Jay Moskowitz said.
Vivage facilities, including Mesa Vista, have done town hall-style group phone calls to try to disseminate information, Moskowitz said.
“These are frontline workers who are coming to work every day when they have a choice not to work and to expose themselves [to the disease]," he said.
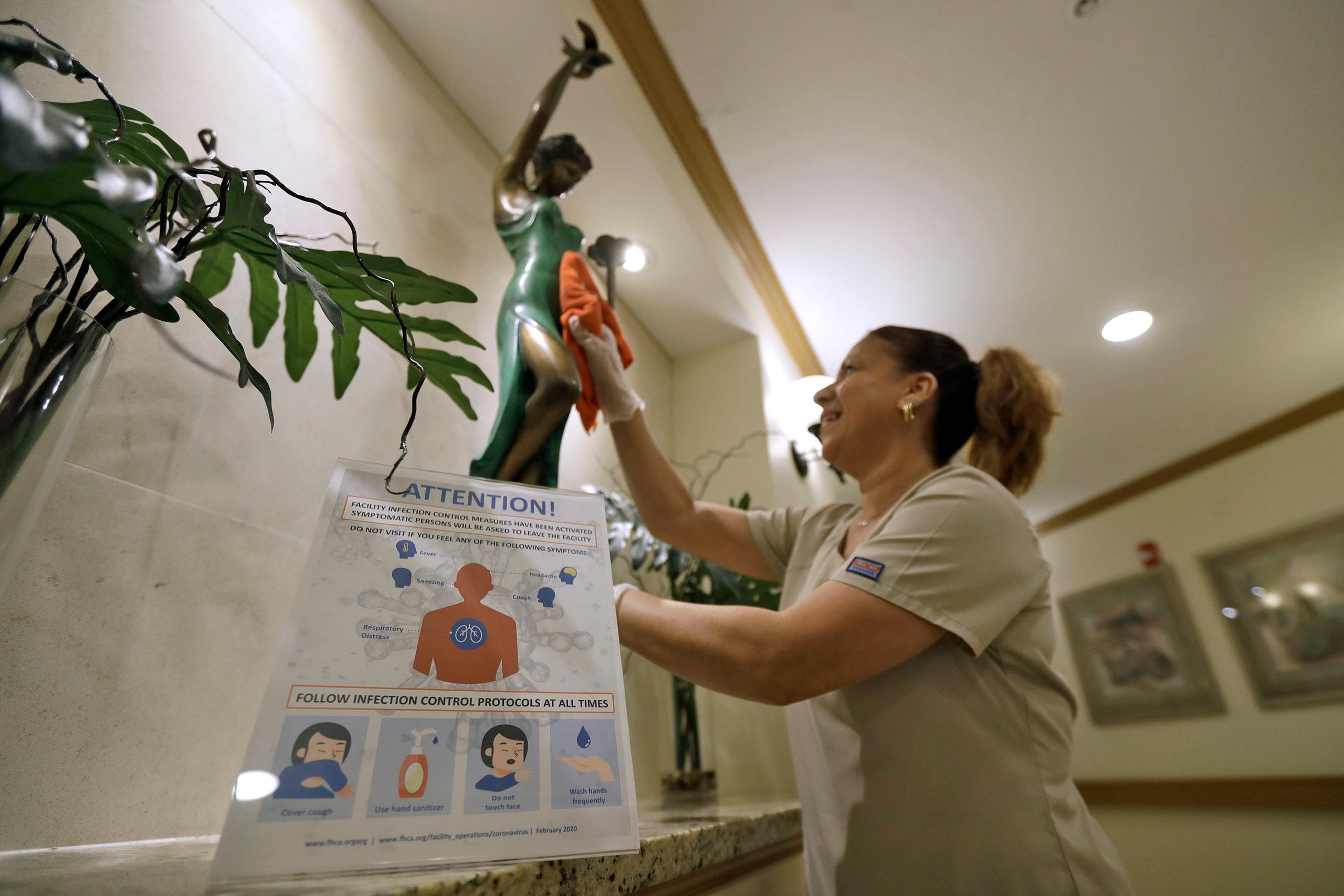
Since March 12, visitation has been closed at nursing facilities along with communal dining and events. Both Gov. Jared Polis and the federal Center for Medicare and Medicaid Services sent down the order in order to keep outsiders from carrying COVID-19 to the vulnerable populations in nursing homes.
The state lab has also prioritized testing for nursing homes, running samples for living residents and post-mortem cases. Some facilities are prioritizing testing for staff to help keep the disease from spreading. This week, Vivage announced that their staff would receive test results within 24 hours and other facilities are rolling out similar testing protocols.
Despite these measures, the disease has continued to spread within the walls of many nursing facilities in both residents and staff. In some cases, the testing occurs long after the outbreak has already worsened.
Administrators at Juniper Village in Aurora decided to test their entire population of staff and residents after several staff members tested positive for the disease on March 27. The test results, announced Saturday, revealed that more than 70 percent of the residents and more than 60 percent of the staff had already been infected.
"The March 14 order limiting visits was critical for reducing exposure in nursing homes, but it's not possible to shield these facilities from all exposure, especially when we know that asymptomatic people can spread the disease,” Ian Dickson, a spokesman for CDPHE, said in an email. "In these facilities, there are a lot of high risk, susceptible people living in close quarters, so it’s a challenging situation even when you have great infection control measures in place.”
The strict visitation measures, while considered the best way to contain the disease, have also had consequences.
Typical nursing-home watchdogs like family members, media and independent investigators known as ombudsman have all been kept out of facilities.
The state licensing board has continued to investigate complaints and outbreaks, but officials report that there is a limited supply of the personal protective equipment those surveyors need to be able to enter the facilities.
Isolation also carries the additional stress for residents and family members.
Sage Lesko from Denver described the anxiety of monitoring the COVID-19 symptoms of her 91-year-old grandmother, Carol Lesko, without being able to visit her at her nursing home, Sunrise at Cherry Creek. Her grandmother’s dementia made isolation stressful for her and doctors believe it made her symptoms worse.
Lesko’s family set up video conference calls, but as more staff members were forced to call in sick due to COVID-19 symptoms it became more difficult to coordinate the calls. Her grandmother died on April 6. A post-mortem test revealed that she was negative for COVID-19 and doctors believe it was the isolation that played a factor in her downward spiral.
“I think some of the hardest parts about it was not being able to be with her especially in those last few days,” Lesko said.
For anyone investigating nursing home deaths, getting information has also been a challenge. The state has been sporadically releasing outbreak information on request. It is set to begin releasing information on nursing-home outbreaks on Wednesdays but information on deaths in nursing homes is tracked at the county level and can only be obtained by calling each county health department.
While nursing facilities and state inspectors insist that they are enforcing the guidelines set out by CMS regarding infection control and screening staff for COVID-19 symptoms, there is no way to monitor what facilities are actually doing. Many facilities don’t know the exact cause of their outbreaks.
Before some families can get answers about their loved ones' conditions, it’s often too late. As of Friday, at least 81 people have died from COVID-19 or a suspected case of it. And with the pandemic still restricting social gatherings, even grief has been put on pause for many.
“My family is pretty small and I couldn’t even console them. I couldn’t hug my mom during all this,” Lesko said. “I think that’s really tough on a lot of families right now, not being able to grieve and mourn together."