Since mid-May, Colorado, like many states, has seen a steady increase in cases of monkeypox. The state’s health department has logged 79 cases total, with 66 of those reported in July alone (though experts say that’s likely an undercount).
The current outbreak of the virus has alarmed members of higher-risk groups and triggered a public health response that is just ramping up. This week, the Biden administration declared monkeypox a national emergency.
The designation opens up grant funding and more federal resources, including ordering more medical supplies for states to use. Gov. Jared Polis on Thursday said Colorado would intensify its response to the outbreak, including hosting more vaccination clinics and increasing access to testing.
“We administer or distribute the extremely limited supply of vaccines that the federal government provides us as soon as we receive them,” Polis said in a statement. “We will continue to advocate for more vaccines and are pleased to hear more are on the way.”
What is monkeypox?
While rarely fatal, monkeypox can cause serious symptoms in those that catch it. People generally experience a flu-like illness followed by a rash or skin lesions or sores that can spread to all parts of the body.
Symptoms typically appear between seven to 14 days after exposure and last anywhere from two to four weeks, according to the Centers for Disease Control and Prevention.
Monkeypox was discovered in populations of monkeys in Africa in 1958. The original source of the disease remains unknown, according to the CDC. Researchers recorded the first human case in 1970.
In the current outbreak, the virus is mostly spreading among men who have sex with other men, a group that includes people who identify as gay, bisexual, transgender and nonbinary. Transmission is not limited to a people who have a specific sexual orientation or gender identity, though.
Monkeypox can spread between anyone through close skin-to-skin contact with sores or any fabrics (clothing or bedding) used by someone who has the disease. The virus can also spread through respiratory secretions.
“I think it is critical that everyone understand what's going on with this virus,” said Dr. Sarah Rowan, an infectious disease specialist at Denver Health who has been leading the system’s response to the outbreak. “There are communities with higher transmission. But anyone can be exposed.”
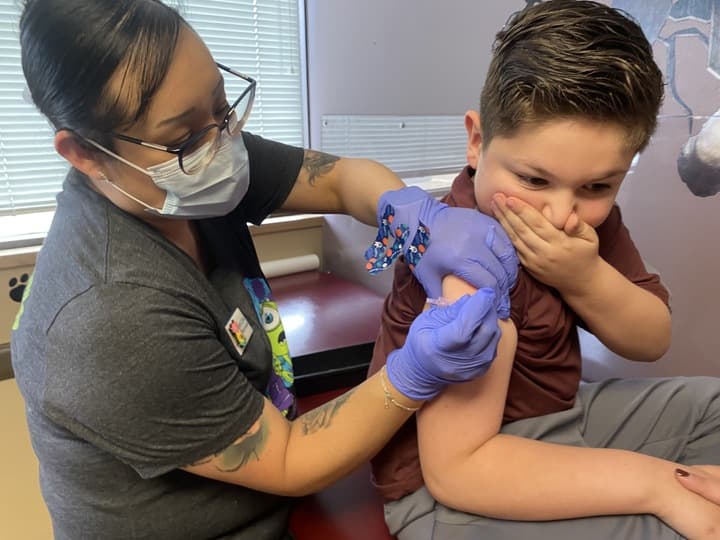
Public health officials say one of the best ways to protect yourself is by getting vaccinated against the disease if you are a member of a higher-risk group. There are also simple precautions you can take on a day-to-day basis.
How to get vaccinated in Colorado
Right now, the main way to get a vaccine is by filling out an online form from the Colorado Department of Public Health and Environment. The form opens and closes as supply fluctuates, so check back frequently if the agency has paused submissions.
Due to low supply, CDPHE is only offering appointments to members of higher-risk groups. In this current outbreak, that list includes men who have sex with multiple other men and people who have had direct exposure to the virus.
Appointments are already fully booked through Aug. 13, so expect a wait.
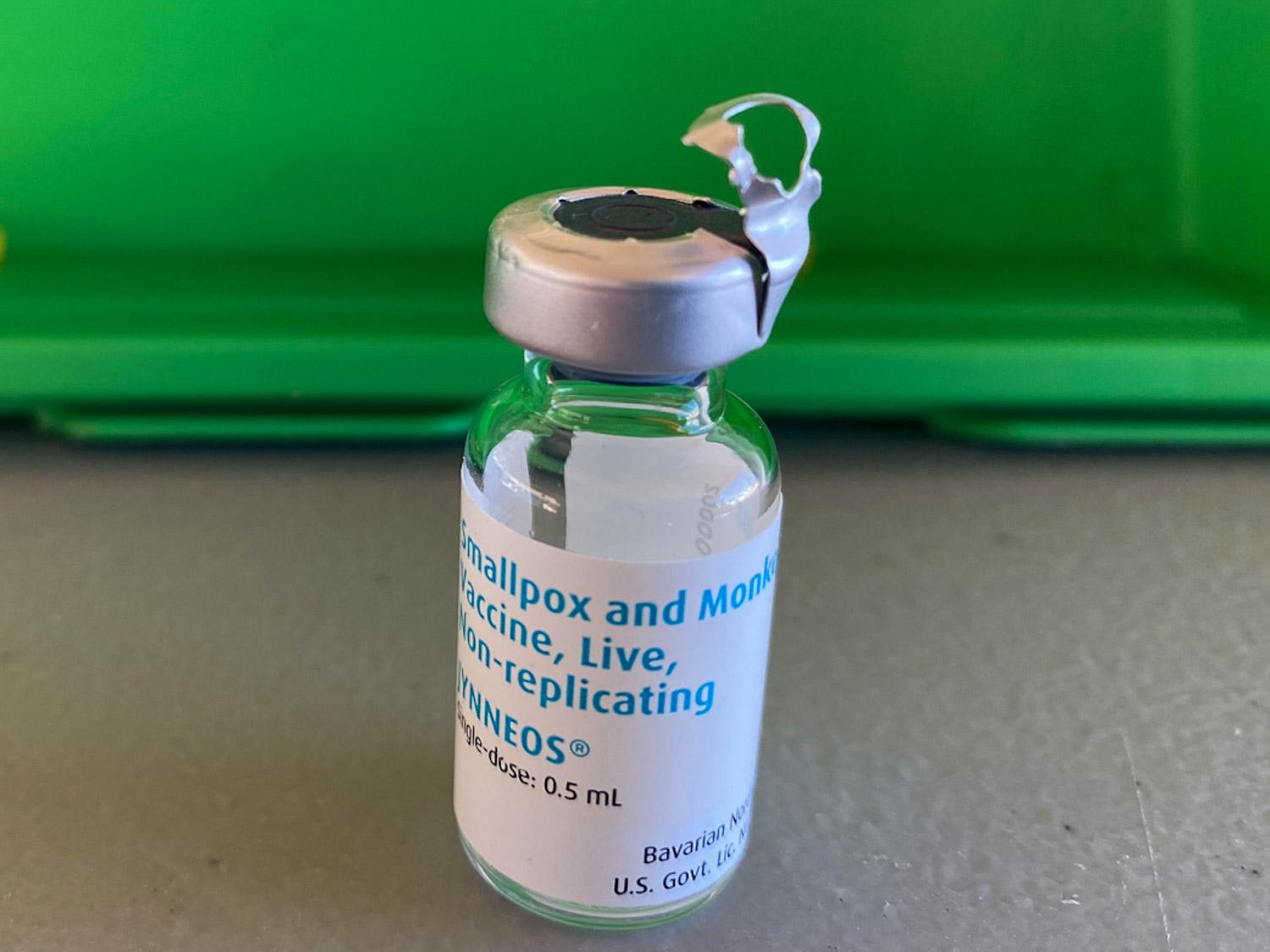
Colorado’s health department has so far vaccinated roughly 2,000 people against the disease. The FDA-approved vaccine, Jynneos, is a two-dose series, but officials have temporarily paused second doses to help get as many people as possible protected with a first dose.
On Aug. 1, Colorado placed an order for an additional 5,000 doses of vaccine from a federal stockpile. Officials say the vaccination wait times should decrease once that arrives.
The state is also expanding the number of places where people can get the vaccine. CDPHE has enrolled more than 30 providers across the state, which will start administering vaccines as supply catches up to demand over the coming months.
How to get tested for monkeypox
The state recommends anyone who is experiencing symptoms of monkeypox contact their healthcare provider to discuss testing.
Many providers, according to CDPHE, can now submit PCR (swab) tests to commercial labs. The state lab has also been processing tests from providers. Results take about 48 hours.
If you don’t have a reagular health care provider or insurance, you can contact a list of public health agencies and sexual health clinics on CDPHE’s website. Most providers aren’t testing people who don’t have symptoms.
If you do have symptoms, let your provider know before your visit. Wear a mask and cover any lesions with clothing or a bandage.
Much like vaccine supply, the state’s testing capacity has been limited for the past several months. And it remains scarce, said Dr. Rowan with Denver Health. Rowan and her team have been doing about 30 tests a week on patients exhibiting monkeypox symptoms since mid-July, she said.
“There's a general consensus that we should be testing more,” Rowan said. “We should be having more negatives so that we know that we are adequately testing and we can get a better sense of how much the outbreak has spread.”
Many urgent care clinics are also offering testing, Rowan said.
If you test positive for monkeypox, you should self-isolate until symptoms go away. There are treatments available.
How to protect yourself against monkeypox
Other than vaccination, doctors and public health experts say there are a few steps people can take to reduce their risk of getting monkeypox. Most of the advice revolves around limiting skin-to-skin contact with people known to have the disease or are showing symptoms.
The CDC says to avoid close contact with people who have a rash that may look like monkeypox. Don’t touch the rash, scabs, clothing or bedding of a person with monkeypox. Don’t kiss, hug, cuddle or have sex with someone who has monkeypox symptoms.
Large gatherings also carry some risk of transmitting the disease. When deciding whether to attend, consider how much close, personal, skin-to-skin contact is likely to occur at the event. Events where people are fully clothed are generally safer and low-risk.
Some businesses have started to impose protective measures, such as closing dressing rooms, to help lower the risk.
Cheyenne Nichols, a tattoo artist in Lakewood, started asking clients to wear masks due to the nature of their work, which involves close skin contact. They also started double cleaning everything in their work area and asking clients who are sick to reschedule their appointment.
“If I notice any lesions on anyone’s hand or face, I will send the person home and ask them to reschedule,” Nichols said. “I think my clients are more comfortable in my chair knowing I’m doing all I can to keep a safe space.”
Guidance is evolving. Public health agencies, including CDPHE, are regularly releasing more information on safer practices for attending gatherings and intimate relationships as the outbreak grows.