In April 2018, 9-year-old Christian Bolling was hiking with his parents and sister in Virginia's Blue Ridge Mountains, near their home in Roanoke. While climbing some boulders, he lost his footing and fell down a rocky 20-foot drop, fracturing both bones in his lower left leg, his wrist, both sides of his nose and his skull.
A rescue squad carried him out of the woods, and a helicopter flew him to a pediatric hospital trauma unit in Roanoke.
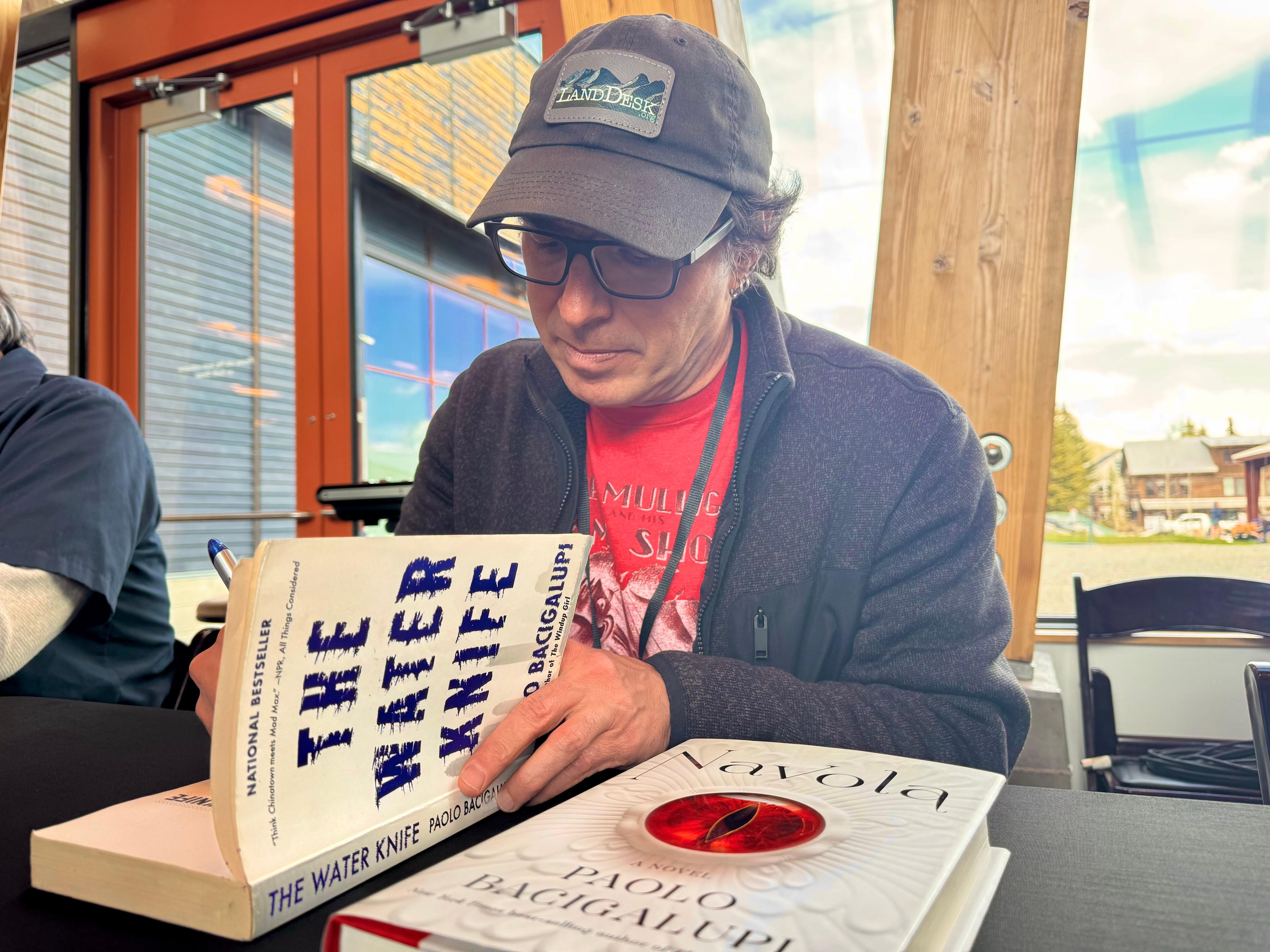
Most of Christian's care was covered by his parents' insurance. But one bill stood out. Med-Trans, the air ambulance company, was not part of the family's health plan network and billed $36,000 for the 34-mile trip from the mountain to the hospital. It was greater than the cost of his two-day hospitalization, scans and cast combined.
"When you're in that moment, you're only thinking about the life of your child," says Christian's mother, Cynthia Bolling, an occupational therapist. "I know I'm being taken advantage of. It's just wrong."
The rising number of complaints about surprise medical bills is spurring efforts on Capitol Hill and at the White House to help consumers. Over and over again, the high cost associated with air ambulance service gives patients the biggest sticker shock — the subject has come up at nearly every Capitol Hill hearing and news conference on surprise medical bills.
Yet air ambulance costs are not addressed in any of the proposals introduced or circulating in Congress. Even a congressional decision last year to set up a panel that would study air ambulance billing hasn't gone anywhere.
"We're doing a disservice to patients if we protect them from hospital bills but bankrupt them on the way there," said James Gelfand, senior vice president for health policy for the ERISA Industry Committee, a trade association for large employers.
The issue came up again Wednesday at a House Energy and Commerce subcommittee hearing where Rick Sherlock, president and CEO of the Association of Air Medical Services (the industry group for air ambulances), was among eight witnesses.
Rep. Ben Ray Luján, D-N.M., sharply questioned Sherlock as to why costs for air ambulance services have risen by 300% in his state since 2006.
"I'm trying to get my hands around why this is costing so much and why so many of my constituents are being hit by surprise bills," Luján said.
Sherlock explained that reimbursements from Medicare and Medicaid do not cover the cost of providing services. So charges to private patients, he told the legislators, must make up that difference.
Air ambulances serve more than 550,000 patients a year, according to industry data, and in many rural areas, air ambulances are the only speedy way to get patients to trauma centers and burn units. As more than 100 rural hospitals have closed around the U.S. since 2010, the need has increased for air services.
More than 80 million people can get to a Level 1 or 2 trauma center within an hour only if they're flown by helicopter, according to Sherlock.
The service, though, comes at a cost. According to a recent report from the Government Accountability Office, two-thirds of the more than 34,000 air ambulance transports examined were not in the patients' insurance networks. That can leave patients on the hook for the charges that their insurers don't cover, a practice known as balance billing.
In 2017, the GAO found that the median price charged nationally by air ambulance providers was around $36,400 for helicopter rides and even higher for other aircraft. The total generally includes the costs for both the transportation and the medical care aboard the aircraft.
Additionally, the Bill of the Month investigative series by NPR and Kaiser Health News has received more than a dozen such bills, ranging from $28,000 to $97,000.
Cynthia Bolling says her insurance company paid about a third of Christian's air ambulance bill, and the family settled this week with Med-Trans, agreeing to pay $4,400 out of pocket.
Reid Vogel, director of marketing and communications for Med-Trans, says he can't discuss a particular patient's case because of privacy rules. But, he adds, Med-Trans works with patients to find "equitable solutions" when their bills are not covered by insurance.
Since nearly three-quarters of flights are for patients insured by low-paying Medicare, Tricare and Medicaid, he says, "providers must shift costs to insured patients."
Yet private insurers usually will pay only an amount close to what Medicare reimburses, which is around $6,500. That gives air ambulance companies an incentive to remain out of network, according to a 2017 GAO report.
"A representative from a large independent provider noted that being out of network with insurance is advantageous to the provider because a patient receiving a balance bill will ask for a higher payment from the insurance company, which often results in higher payment to the air ambulance provider than having a pre-negotiated payment rate with the insurer," the GAO found in its report.
Sherlock, of the air transport trade association, disputes the report's findings, saying his members are actively trying to be in network in more places, although he can't provide any specific numbers.
"I think that everywhere they can, they're incentivized to be in network," he says.
States are hampered in their efforts to ease the strain for residents.
The Airline Deregulation Act of 1978, which was intended to encourage more competition, prohibits states from regulating prices for any air carrier, including air ambulances. What's more, many large employers' health insurance is not governed by states but regulated by the federal labor law known as ERISA.
So a remedy likely has to come from Congress. And it has proved to be a heavy lift.
For example, the committees that deal with regulation of the air industry — the Commerce Committee in the Senate and the Transportation Committee in the House — don't make health policy or regulate health insurance.
Last year, some lawmakers sought to let states regulate air ambulances with a provision in the bill reauthorizing the Federal Aviation Administration.
But that measure was ultimately eliminated. Instead, the bill called for the creation of an advisory committee to study air ambulance prices and surprise bills.
"The air ambulance lobby did a very good job playing defense during FAA authorization," says Gelfand.
The panel, which was supposed to be formed within 60 days of the law's enactment date — Oct. 5, 2018 — still has not been created.
Representatives from the air ambulance industry don't think congressional action is necessary, although they are calling for higher reimbursements from Medicare.
Chris Eastlee, vice president for government relations at the Association of Air Medical Services, says his group does not favor more congressional regulation of prices but would support mandatory disclosure of costs to the secretary of the Department of Health and Human Services. Greater transparency, Eastlee's group argues, will help companies negotiate more in-network contracts.
A fix for surprise bills that is supported by some researchers and advocates would require every health care provider within a medical facility to accept any insurance plan that contracts with that hospital. It might also help bring down air ambulance bills, says Loren Adler, associate director of USC-Brookings Schaeffer Initiative for Health Policy.
It would avoid the situation where someone picks an in-network hospital only to find out that a surgeon or anesthesiologist at that hospital doesn't take the patient's insurance. Air transport should also be included in the rule, Adler says.
"It's the exact same situation as with the out-of-network emergency facility rates," Adler says. "The same solutions should apply."
Gelfand suggests also that the House Ways and Means Committee require air ambulance companies seeking to participate in Medicare to always charge in-network rates.
That would require only a small tweak of the legislative language, as Gelfand sees it. "Every proposal that includes something to address surprise bills for emergency care, all you [would] have to do is add in the words 'air ambulances,' " he says.
Right now, the closest any surprise-billing proposal has come to addressing air ambulances is a draft legislative plan on medical costs from Sen. Lamar Alexander, R-Tenn., and Sen. Patty Murray, D-Wash.
Their plan would require that bills for air ambulance trips be itemized to show both medical charges and the transportation charges — so patients and health plans can understand them better.
Kaiser Health News is a nonprofit, editorially independent program of the Kaiser Family Foundation. KHN is not affiliated with Kaiser Permanente.
9(MDEyMDcxNjYwMDEzNzc2MTQzNDNiY2I3ZA004))