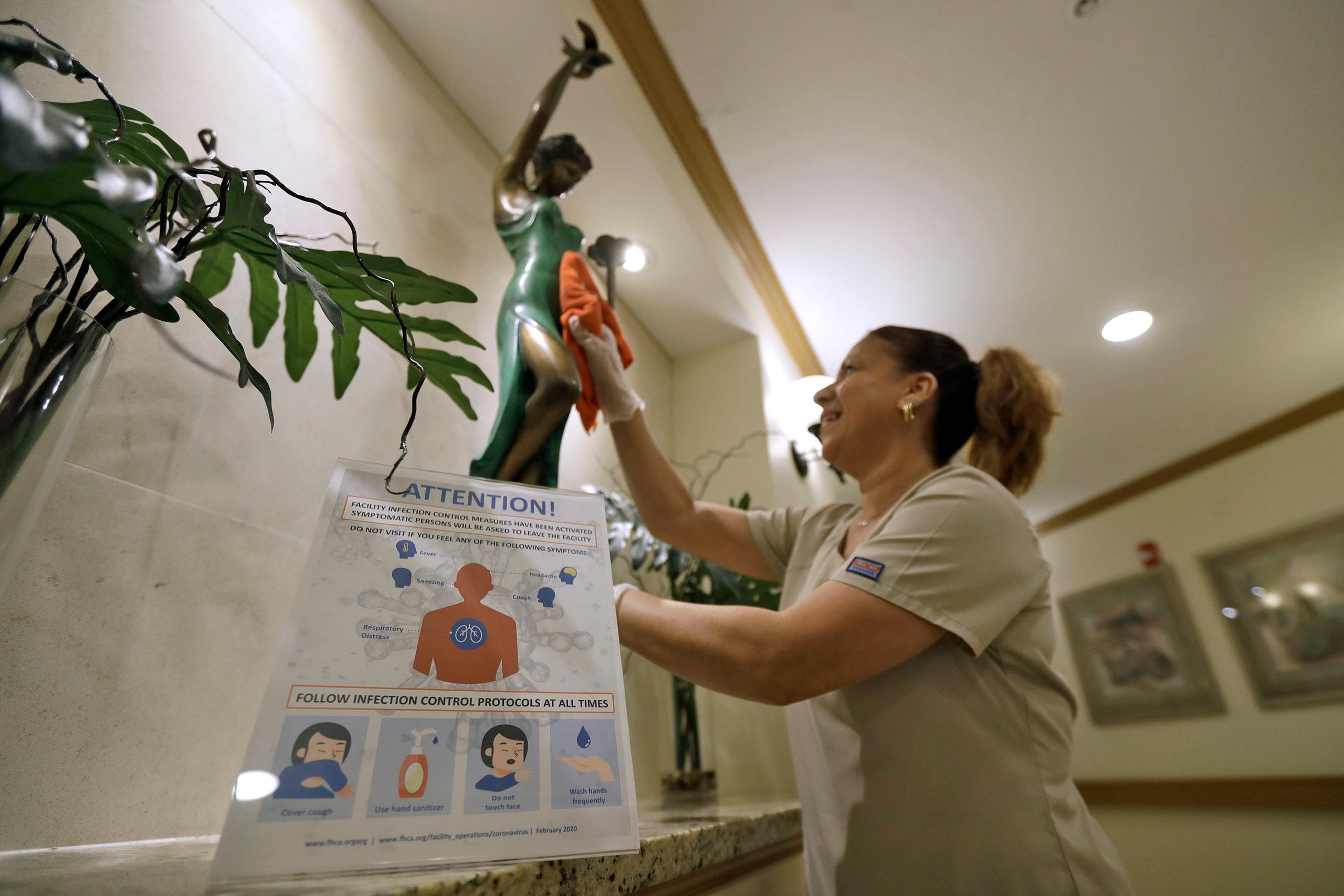
Linda Allour’s dad is in a nursing home in Longmont. When she visited him just days ago she was pleased to see that the facility was screening visitors at the door. She filled out a questionnaire about her recent travel and whether she was experiencing any symptoms of a cold or the flu.
“I thought they did an excellent job,” Allour said. “I don't feel that nervous about it because when you're in a facility like that it’s not uncommon for bacteria and viruses to be there anyway, regardless of any type of outbreak. So, I feel they already watch for that.”
Last fall, when her dad was at another facility, he and his roommate got the flu. Allour’s dad was transported to the hospital, and his roommate died. Allour said that was scary, but they’d made it through. Then this week as coronavirus started to spread in Colorado, she became concerned about visiting her dad.
“I'm nervous about continuing to visit my dad since I own a business, and I have such a large contact with the public,” said Allour, who owns a Daylight Donuts shop in Dacono. “I'm afraid of my exposure to him because everyone at the nursing home has a compromised immune system.”
As the risk to the elderly from the coronavirus became all too real with Colorado's first death — of a woman in her 80s who lived on her own in El Paso County - the state's nursing homes and other facilities for the elderly were already tightening restrictions and making changes to protect residents.
Among them: screening staff for signs of illness, re-educating staff and residents on proper hand washing techniques and proper cleaning protocols, and screening even familiar visitors like Allour to make sure they don't pose a risk.
“Our goal is ‘not one patient affected,’” said Jennifer Brown, director of nursing at a Grand Junction facility called The Center at Foresight. “Every day we meet to revise and add things that come up because infection control isn't just wearing protective equipment or hand-washing.”
On Wednesday, Gov. Jared Polis issued an emergency declaration that called for restricting visitor access to facilities that house and serve older people. The order requires facilities to devise alternative means of non-contact visitation, to require proof of screening for the virus for any essential third parties who must get into the building, and to keep a log of anyone who came in so that future infections can be investigated.
There have been 77 confirmed cases of COVID-19 in the state and state officials suspect community spread of the virus. Dr. Jeff Wallace, a geriatrician at the Multidisciplinary Centers on Aging at CU Anschutz Medical Campus, said restricting access early is one of the things Colorado has learned from the outbreaks at nursing facilities in Washington state that left 19 dead and dozens infected.
But, these facilities can be difficult to protect. They house a highly vulnerable population that needs contact with the outside world in the form of staff and family.
“Care providers come and go. From the medical staff to the hands on nursing assistants and nurses in the building, there is going to be some in and out throughout the buildings,” Wallace said.
If staff do become sick many, and especially nurses aides, may not have paid time off that allows them to take the time they need, Wallace said.
“These are not great paying jobs. These are stressful jobs, and if there are other factors going on in their lives that make it hard for them to come to work it's going to be a big strain,” Wallace said. “Government policies and announcements included having paid leave for these people so that they can take care of themselves and not be out for extended periods.”
Read more: How does COVID-19 spread?
Polis’ emergency rules included a measure that will require employers to offer paid sick days to hundreds of thousands of service and hospitality workers. The rule will affect an estimated 15% or more of the state’s 3.1 million workers, according to state projections.
Vivage Senior Living, which has 30 nursing and assisted living communities in Colorado started restricting visitors after Polis’ announcement. Jay Moskowitz, president and CEO, said that keeping patients safe is the number one priority.
“Our top priority is to protect the safety and welfare of our elder that we serve in these communities,” said Cynthia Coenen, chief medical officer at Vivage senior living. “We have heightened communication to residents, their families, our staff. We are daily calls with all of our communities in terms of providing them with the latest information from CDPH or CMS [Centers for Medicare and Medicaid Services].”
Nursing homes and assisted living facilities receive guidance from the state health department, CMS and the Centers for Disease Control and Prevention. Facilities are required to have infectious disease plans among other emergency preparedness plans.
Prevention has been the focus, but keeping patients calm and comfortable is also important. At Vivage, patients and their families are encouraged to communicate through Facetime and over the phone during the restricted hours, and there are still enrichment activities taking place, Coenen said. In the case of end of life or an emergency, Coenen said the facility will make sure that family have access to their loved one.
If the virus does make its way into a facility, then the next step is to detect it quickly. Wallace said he supports the efforts to expand testing in the state.
“We're still not there, and we're still having to decide who should really get the flu test and who should get the Corona test,” Wallace said “It'd be nice if we just did it all upfront, and in Washington they are doing that now. So, if you have respiratory symptoms in a nursing facility in Washington, they check for the Coronavirus first.”
Wallace acknowledged that there are limitations to getting Coronavirus tests, and said that the testing landscape could change quickly.
“I'm confident that this is not going to be a disaster in the nursing homes,” Wallace said. “I hope I won't be regretting that statement a month from now. I do think we're going to see more cases, but honestly, I have been impressed by the resources and effort that I've seen in the last week, both on the local, the state and increasingly on the federal level to bring the resources and do the planning.”