For $100 and a quick stick of a needle, you can get a test that will tell you whether or not you have had COVID-19.
The antibody test, also known as a serological test, looks for antibodies in the blood. The Y-shaped molecule is produced by the body's immune system when it fights off infection. Again, the important distinction is that this test doesn’t tell you if you are currently infected.
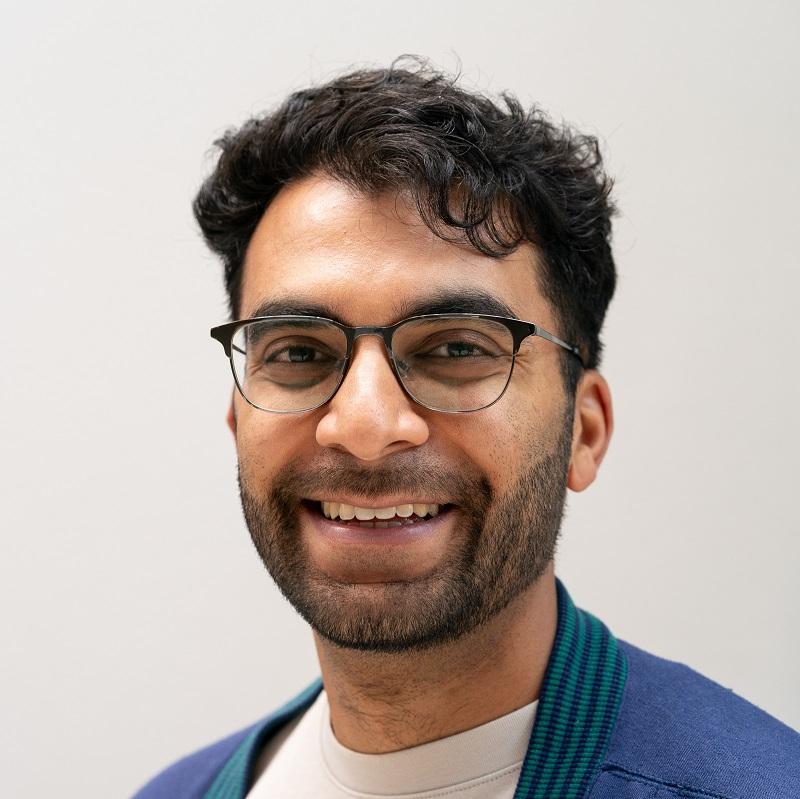
“There will hopefully be a lot of research and guidance about what it means, but the only thing it means today is that you have been exposed to the COVID-19 virus,” said Dr. Richard Zane, chair of the Department of Emergency Medicine at the University of Colorado School of Medicine.
Antibody tests were touted early on as a way to reopen society and catch coronavirus cases missed by the PCR test, which looks for active infection in the nose or throat. Until recently, the tests were plagued by inaccurate results.
In late April, researchers tested the accuracy of 14 antibody tests and found that most did not deliver as advertised. Until that point, the Food and Drug Administration had not been evaluating the tests for accuracy. It then stepped in and required companies to prove their accuracy or the tests faced removal from the market.
“Over the course of the last weeks, the difference has been the FDA getting involved and the [Centers for Disease Control and Prevention] issuing guidance on the use of antibody testing and how to test,” Zane said.
In the interim, it was a confusing landscape for antibody testing. Established companies competed with unapproved tests made by unknown companies. And meant that consumers were in the dark about accuracy and what the results meant.
Testing reliability has since come a long way.
Researchers at the University of Colorado Hospital at the Anschutz Medical Campus, developed a “homegrown” antibody test with a specificity of 99.3 percent — defined as out of 1,000 tests, seven people will get a false-positive result.
In evaluating antibody tests, two measures are important: specificity and sensitivity.
“The sensitivity is what is the rate of false negatives. Meaning when I say the test is negative, what's the rate of it being truly negative,” Zane explained. “And then the specificity is what's the rate of false positives. When I say that a test is truly positive, is it truly positive? So a perfect test is a 100 percent sensitive and a 100 percent specific.”
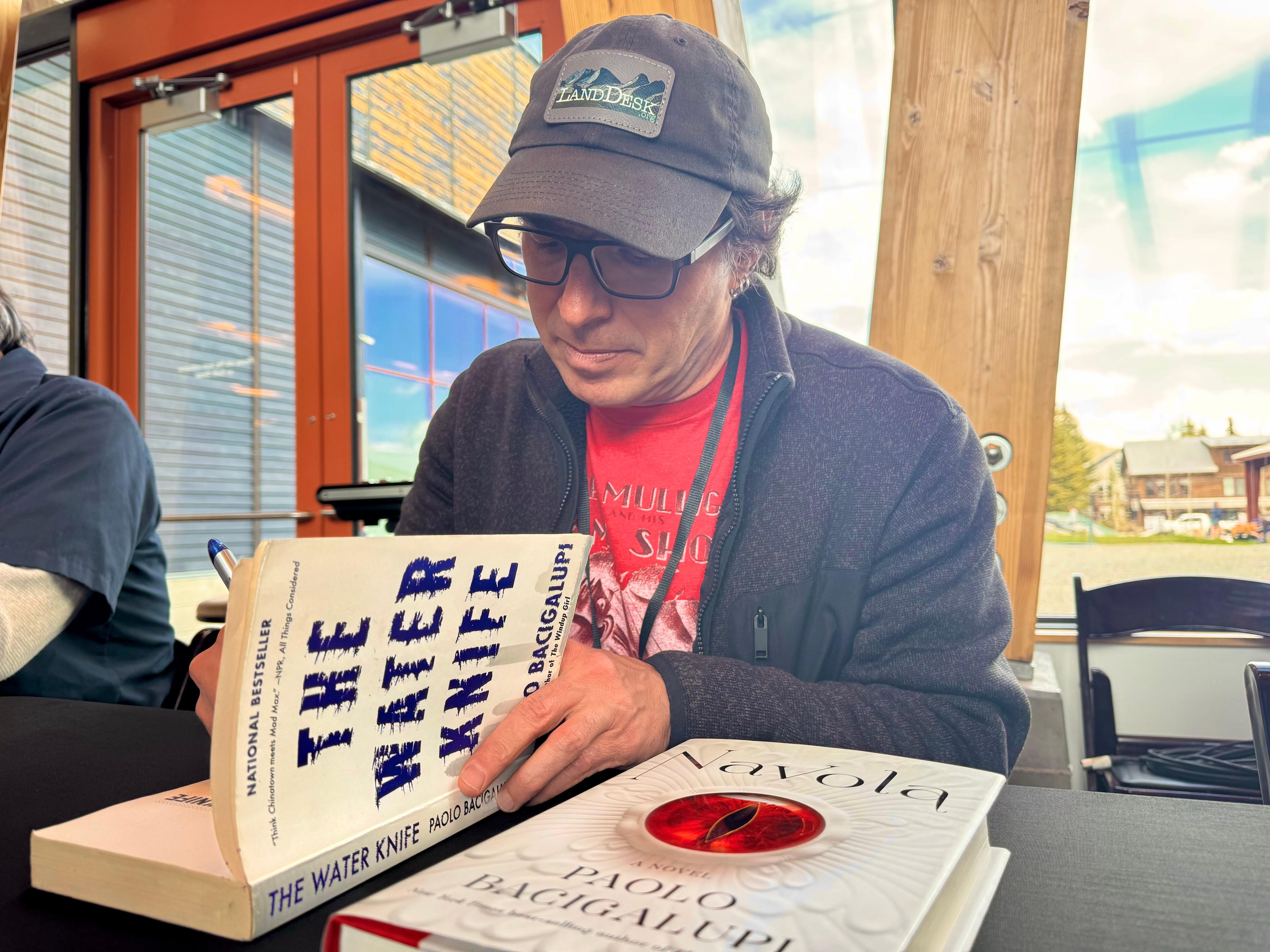
Dr. Brian Harry, medical director of special chemistry at the UCHealth University of Colorado Hospital and an associate professor of pathology at the CU School of Medicine, was one of the researchers who developed the antibody test.
“So, you know, for those seven people that it is concerning, right?” he said. “From a testing perspective, that is an excellent number.”
If the test gives too many false-positive rates then people may think they’re immune to the virus when they aren’t. They may later put themselves in danger by abandoning social distancing and other protective measures. Which also leads to other questions that so far aren’t answerable: how long do the antibodies from COVID-19 last? And how well do they protect someone from reinfection?
“We have every reason to think that the immune system and the antibodies produced have some power against the invading virus,” Harry said. “People are skeptical, however, to make the claim that there's going to be immunity conferred from the antibodies that you can detect. And I think that mainly comes from the really widespread impact of COVID-19 and concerns about how the antibody test is going to be used.”
Widespread immunity in a community would allow governments to relax social distancing measures. But, scientists still don’t know how long the immunity to COVID-19 lasts or if it will protect from reinfection. Some diseases, like tetanus, do not result in immunity.
Countries like Germany, Chile, the UK and the U.S. have floated the creation of “immunity passports.” In theory, people who have immunity to SARS-CoV-2, the virus that causes COVID-19, would be able to travel more freely and go back to work or school.
“One other really important piece to this is that viruses can mutate, right? So, you get an influenza vaccine every year because it's a slightly different strain,” Harry said. “We don't know how the virus is going to change over time and whether or not people who made antibodies this year are going to be protected next year, for example.”
How long it will take for scientists to understand immunity to COVID-19 is not clear. So far, there haven’t been many reports of reinfection, which is another indicator, he said.
If the patient’s antibodies neutralize or make the virus harmless, then researchers know the antibodies are effective. But how long these antibodies last will take time to tell.
“You might be safe where you may not get it again, but it's likely just with most respiratory viruses, it's temporal,” said Dr. Michelle Barron, medical director for Infection Control and Prevention at the University of Colorado Hospital. “So you have some protection from getting the infection again for like a month or two, and then it goes away.”
The idea of immunity passes also has the potential to be a breach of privacy or create a kind of stratified society where those with immunity have access to work, child care, entertainment, friends and family — while those without are stuck on some form of lockdown. The temptation to gain immunity through purposeful infection would be strong.
In the meantime, Zane said scientists can use the antibody test to understand population infection rates, “whether they're socioeconomic groups or groups of people with certain underlying conditions or certain geography.”
UCHealth used antibody tests from other companies to test their health care workers and found that just 2.3 percent of those tested had COVID-19 antibodies. As of June 3, the hospital tested over 12,00 people in Colorado and 3.7 percent of those tested positive.
The tests are also used for convalescent plasma, a treatment that is currently under investigation by hospitals across the country. The plasma from a recovered patient has shown promise in improving an ill COVID-19 patient.
If you choose to get an antibody test, be sure that it’s offered through a reputable source like a hospital or doctor’s office. There are tests online that may not be reputable. Additionally, you should check that the test you take has a specificity of at least 98 percent — the higher, the better. And remember, even if you test positive, that doesn’t mean you’re in clear just yet.
“It’s imperative to remember we are still in the midst of a pandemic, and my message to everyone is: Don’t let your guard down. Don’t change your behavior,” Barron said. “Continue to practice physical distancing, wash your hands often and wear a mask when appropriate.”