Cases of the respiratory disease tuberculosis are increasing in Colorado.
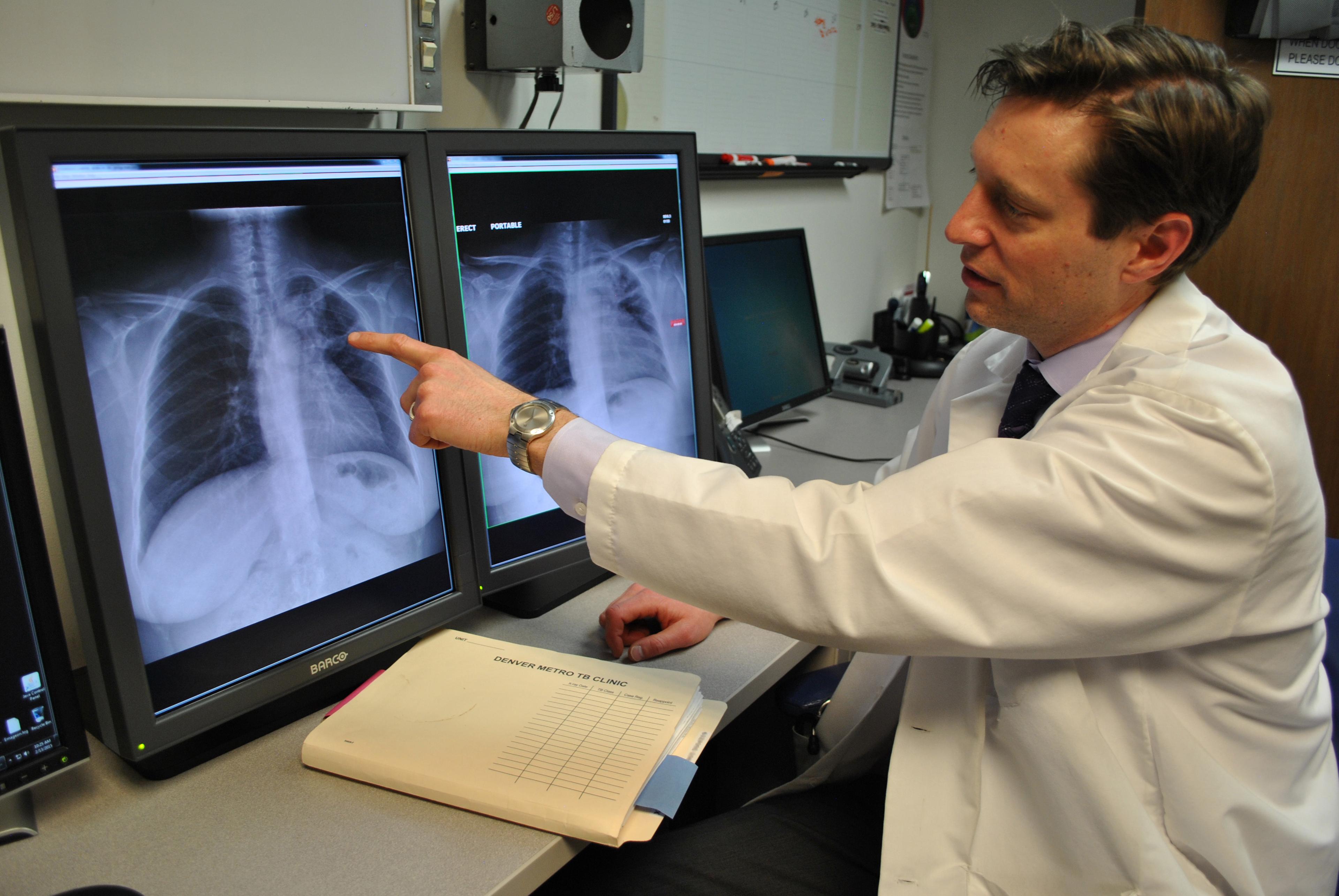
Tuberculosis is a potentially serious infectious bacterial disease that mainly affects the lungs.
After a decade-long drop in cases, Colorado has seen a nearly 60 percent increase in cases this year from last: There were 57 reported cases last year compared with 84 cases this year.
“The numbers of cases are low overall, but we do know that TB is a priority. It's a challenging disease to treat,” said Dr. Rachel Herlihy, the state epidemiologist. “So we are certainly seeing an increase over the last couple of years.”
Eight cases this year were found in patients younger than 18 years old. Two people in total have died.
”It just highlights that just when people do develop active tuberculosis, how serious it can be that there were two deaths reported for 84 cases,” said Dr. Larissa Pisney, an associate professor at CU Anschutz.
What’s driving the trend? It’s not clear.
“One theory is just around the pandemic itself and people not seeking health care and providers potentially being distracted by COVID from thinking of other diagnoses,” Pisney said. “This isn't unique to Colorado and this is being seen in many parts of the country, and again, it'll probably be a year or two before we really know the drivers for it.”
“We don't know if this is just sort of a blip for a single year or if we could potentially see increases for a longer period of time,” Herlihy said.
Before the pandemic, the state’s five-year average number of cases per year was about 70, Herlihy said. During the pandemic years, that figure was typically 50 to 60 cases.
Providers can screen for TB and treat it before it becomes a serious case.
TB is spread via airborne particles. Those at highest risk are people who have lived or have had extended travel to countries that are at higher risk for TB as well as those who live in communal settings.
Tuberculosis is caused by a bacterium called Mycobacterium tuberculosis, according to the CDC. The illness usually attacks the lungs, but it can also infect other parts of the body like the kidney, spine, and brain.
Not everyone infected with it gets sick. If not treated properly, however, TB disease can be fatal.
Symptoms can include a bad cough that lasts three weeks or more, chest pain, or coughing up blood or sputum — phlegm from deep inside the lungs.
Other symptoms include weakness or fatigue, weight loss, a lack of appetite, chills, fever, and night sweats.
Pisney said, given the uptick in cases, providers should be on the lookout for it. It can be detected with a test and treated with antibiotics.
“There is treatment available to ensure that those people will not go on to develop an active infection,” said Herlihy, adding there’s also treatment for people with active infection. “The treatment courses are long. It's complex, and extend multiple months of treatment for both a latent infection and active disease,” she said.
The CDC estimates the rate of TB in the United States to be about 2.5 per 100,000 persons.
There is substantial overlap between the risk factors for severe TB disease and severe COVID-19 infection, Herlihy said. However, the available evidence suggests that having COVID may not put you at greater risk for developing TB.









