Back in the early days of the pandemic, Colorado’s nursing homes were among the first to be ravaged by the novel coronavirus. It was clear that the elderly were more vulnerable to the virus but critics also blamed inadequate testing, a lack of treatment options and a shortage of personal protective equipment, or PPE, for failing to save more lives.
Then, testing at facilities ramped up, researchers discovered better treatments and nursing homes began acquiring more PPE.
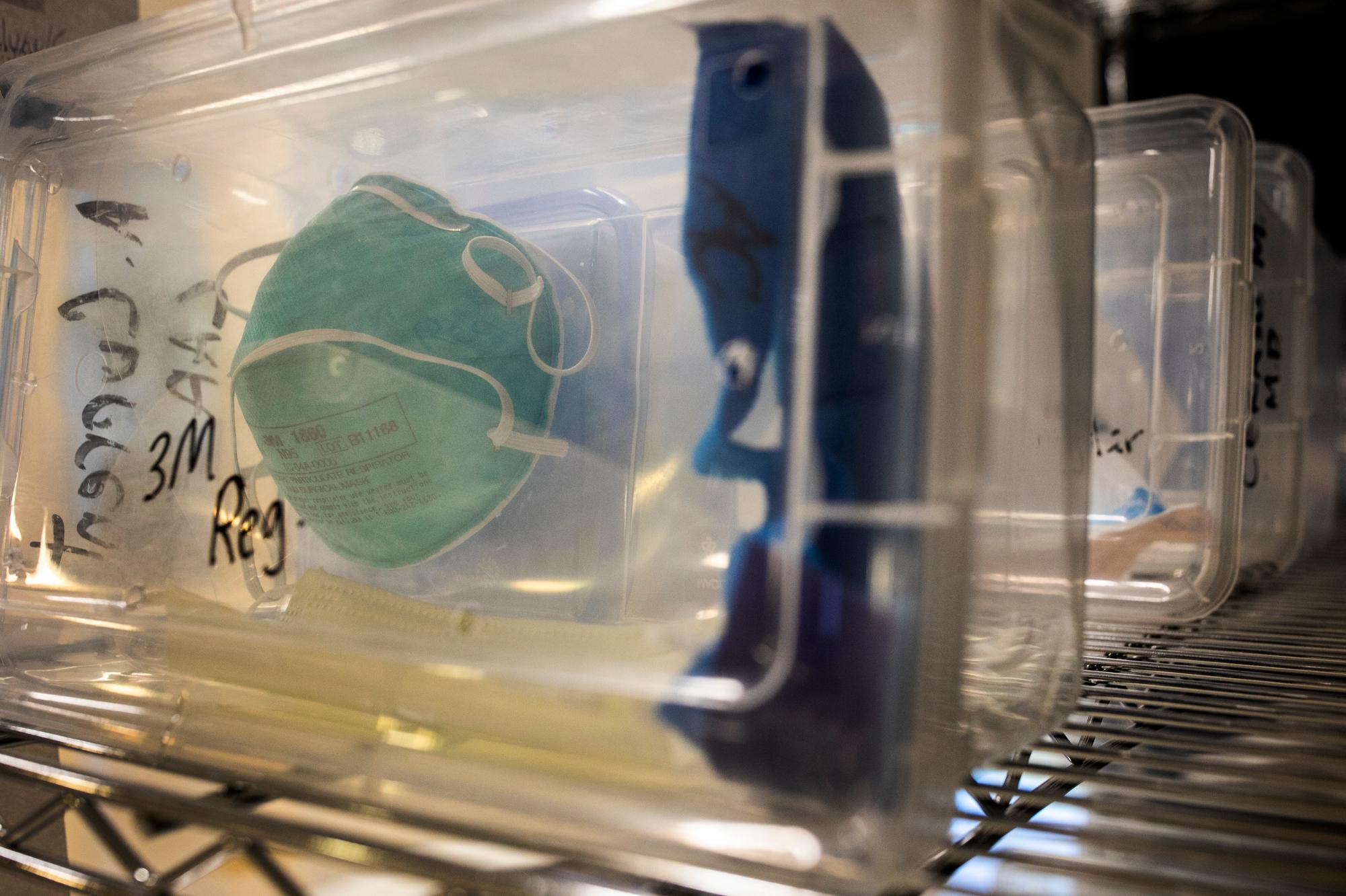
But a new report by Colorado Public Interest Research Group, or CoPIRG, found those same facilities are now experiencing major shortages of PPE, just as COVID-19 cases and hospitalizations are on the rise. The report characterized the problem as worse than earlier on in the pandemic and revealed shortages of masks, gowns, gloves and eye protection, among other supplies.
"It's maddening to think that we are so far into this pandemic and we're still struggling to get the kinds of critical supplies to some of our most vulnerable populations,” CoPIRG’s Danny Katz said.
The report also identified major PPE shortages in nursing homes nationwide, not just in Colorado.
Katz said the lack of PPE in nursing homes affects everyone. Without enough masks, gowns and gloves, employees may feel it is necessary to re-use them as they move from resident to resident, increasing the odds of spreading the coronavirus.
“We're not only endangering the lives of the people in those nursing homes and ... the people who work there, but the folks who work there are also going to be interacting with a lot of us as well,” Katz said.
The most pressing concern, according to the report, is a lack of N95 masks, considered the gold standard for reducing transmission of the virus. CoPIRG surveyed nursing homes in late August and found about 20 percent of nursing homes reported having one week’s supply or less and about 8 percent reported having none.
Home health care providers have complained about the high cost of supplies due to problems with the supply chain and increased competition.
The group urged federal officials to fully implement the Defense Production Act to make more PPE available and it recommended multi-state consortiums to reduce competition and lower prices.
CoPIRG also released a guide for families who have loved-ones in nursing homes or are considering moving into one. It includes questions to ask these facilities about COVID-19 and their supplies of PPE.








