Recent research from the University of Colorado says the medical workforce is facing a crisis-level shortage in primary care doctors. The problem is particularly pronounced in rural areas, which have a difficult time recruiting and retaining doctors to practice.
But Mark Deutchman is working to change all that, one rural clinic at a time.
During a slow afternoon at the UCHealth Primary Care Clinic in Estes Park, Deutchman and another doctor practiced giving each other ultrasounds, one lying on an exam table and the other using a compact new handheld device connected to a tablet computer.
Deutchman is a physician at the University of Colorado Anschutz Medical Campus. He regularly visits small town clinics to train doctors in the use of emerging technologies. He also directs the Rural Track Program at Anschutz, and a big part of the reason he facilitates such training is so the clinics can return the favor for his students.
“[They] take advantage of having their physicians that they’re learning from have the ability to teach them in these different technologies,” Deutchman said.
A lot of Colorado is made up of rural or frontier areas, and that means a lot of Colorado is facing a primary care shortage.
Deutchman said two-thirds of Colorado’s 64 counties are “rural” or “frontier,” and essentially all of them are facing a primary care shortage.
The rural program at Anschutz started in 2005 as a way to encourage more medical students to move into primary care with the eventual goal of placing them in rural posts. But convincing younger doctors to move to rural places to practice is a persistent challenge.
Colorado’s rural areas have less than 10 percent of the state’s physicians, and rural job openings for doctors often take years to fill. A recent study co-authored by Deutchman claims medical schools around the country overestimate the number of graduates going into primary care by almost double. His research shows few new doctors are choosing to practice primary care and are therefore unavailable to help close the yawning gap in rural health care access.
The study suggests the method commonly used by medical colleges to report primary care graduates lumps in specialists such as internists and pediatricians who more often end up practicing outside of traditional primary care roles.
The researchers followed the careers of nearly 18,000 medical school graduates from 14 different U.S. institutions. Of those graduates, about 22 percent actually ended up in primary care jobs. The authors of the study say traditional reporting processes vastly overestimated the number who would end up as primary care docs, at 41 percent.
A new methodology provided by Deutchman and his fellow researchers was much closer in its prediction, estimating about 17 percent of the graduates would wind up as primary care physicians, a slight underestimate.
Michael Dill, who studies the physician workforce at the American Association of Medical Colleges, expressed concerns about the premise and findings in Deutchman’s study. Through increased class sizes and the opening of 30 new medical schools in the U.S. since 2006, the sector is “indeed adequately addressing the primary care shortage, as well as the broader shortage,” Dill said in a statement.
But Deutchman said the evidence in rural areas tells a different story. He said the doctors being turned out by these new colleges are far more often moving into higher-paying specialty areas of medicine after their residencies in mostly urban communities.
Lots of rural doctors are nearing retirement, so time is of the essence when recruiting the next generation.
Not only is the primary care problem not being solved, he said, but it’s also about to accelerate. He said a large portion of rural doctors are nearing retirement, and that that will soon expose a much wider shortage than what the medical workforce is currently seeing. Additionally, Deutchman said replacing those physicians might not be a one-for-one trade — as younger generations demand a greater work-life balance.
“People don’t want to work 24/7, 365, and medicine is more complicated than it used to be,” Deutchman said. “We know that it takes more than one new physician to replace a really active, dedicated, retiring physician.”
Deutchman and his colleagues say hiring more nurse practitioners or physician assistants in teams with new rural doctors could stretch the number of patients served while respecting employee lifestyles. In the meantime, they argue telehealth could do a lot to help the rural health provider shortage, but it’s not enough to close the gap and it’s no substitute for physical interaction with a physician.
At CU Anschutz, Deutchman’s rural track program is a relatively small elective within the medical school, attracting about 10 percent of medical students there. But, though their numbers are small, aspiring young doctors in the program say they feel they learn the practical skills needed for basic medicine long before many of their colleagues do.
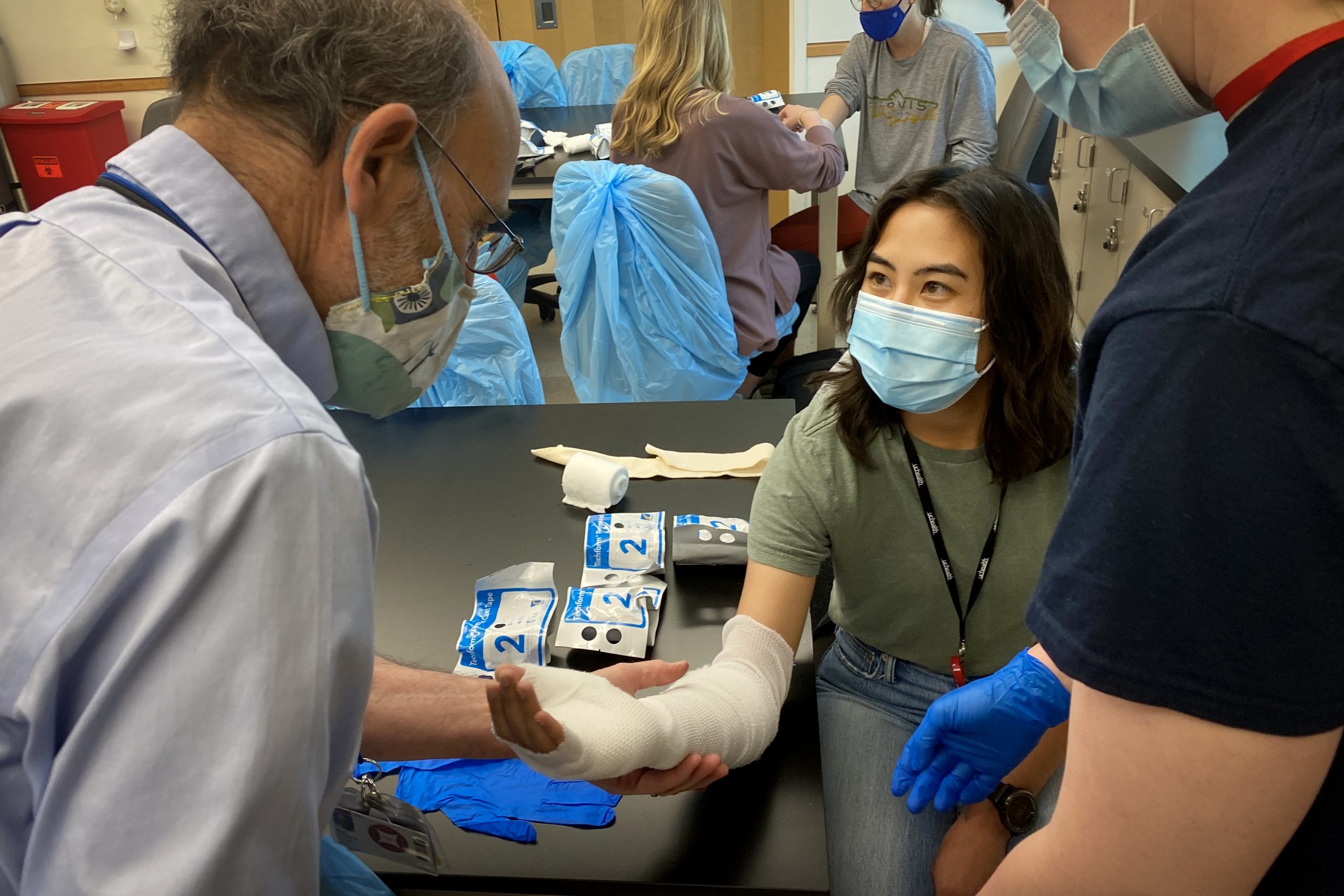
A recent in-person workshop on campus had students wrapping each other’s arms in real casts before learning to saw them off. Coco Wham, a 27-year-old medical school student, said attending a rural immersion week in Trinidad last year convinced her she wanted to be a small-town doctor.
Wham said the rural track tries to prepare medical students for managing their eventual work-life balance, even prepping them to enact strong boundaries when seeing patients in their local grocery store. Though, she said learning to accommodate those challenges is well worth the effort in order to be an important figure and changemaker in a community.
“I know I want to be a really good doctor, but I also want to be a really good person,” she said. “I want to have an impact that goes beyond just being a healthcare provider.”