
To start 2021, Sara Kollman, a top nurse administrator with Kaiser Permanente based in Colorado, found herself in a place she wouldn’t have imagined a year ago: working as an ICU nurse in a hospital in southern California.
“Never in my 30 years have I walked through the ICU and seen so many people that aren't expected to live, that are on their bellies to help oxygenate their lungs and they're just very, very, very ill,” she said.
It’s been exhausting, emotional duty. She describes meeting a mother and her daughter, a similar age to her own, coming in for a final farewell for another family member.
“It was a rough day,” she said. “It just really hit me hard.”
In her regular professional life, Kollman is Chief Nursing Officer for Kaiser Permanente Colorado. But when Kaiser's California system put out the call for help, she volunteered. Kollman was assigned to the hard-hit LA region, at Downey Medical Center, southeast of downtown.

There, she described an intensive care ward overflowing with COVID-19 patients, many on ventilators, fighting for their lives, many not making it.
On one recent day, the hospital brought in a second morgue trailer to handle the many dead bodies
“Because the internal morgue and the current morgue trailer were completely full,” Kollman said. “There was no more room.”
Kollman is one of Kaiser Colorado’s 50 frontline providers who stepped up. They’re filling in for their California counterparts, who are overworked, overwhelmed and exhausted by a tsunami of cases.
She says, like so many nurses, stepping up to care for others is part of her identity.
“Being a nurse is part of my DNA and that's what we do, especially in the ICU. You run to the coding patient. You're there to assist as soon as someone starts to deteriorate or become unstable,” she said. “There was no question for me about going to help. That's where the need is and that's where you go.”
Hospitals are hitting their breaking points
The need for health care back-up reflects a tough reality. Many U.S. hospitals hit a breaking point as COVID-19 hit record levels.
Patti Harvey, a senior vice president with Kaiser Permanente Southern California, says certain ICU providers are in especially high demand, like medical assistants and respiratory therapists.
“We have really been, in southern California, battling this surge since November,” Harvey said. “And by the time Christmas and the holidays rolled around, we knew that this was not going to be a short-term situation.”
Dr. John Eisenach, a Kaiser Colorado anesthesiologist, also volunteered. He got assigned to another hot zone, in Riverside, east of LA. His job is to help a lead doctor supervise a team of other ICU physicians.
His time working in Colorado hospitals with COVID-19 patients has given him plenty of relevant experience, including in the critical procedures that involve ventilator support, inserting tubes to help people breathe. He says treating patients during the pandemic has been eye-opening.
“I've never seen so many people of so many ages with relatively few or no medical problems come to the ICU in extreme distress with respiratory failure and not all of them actually can make it,” said Eisenach, who works at Good Samaritan Hospital in Lafayette and Denver’s St. Joseph’s Hospital.
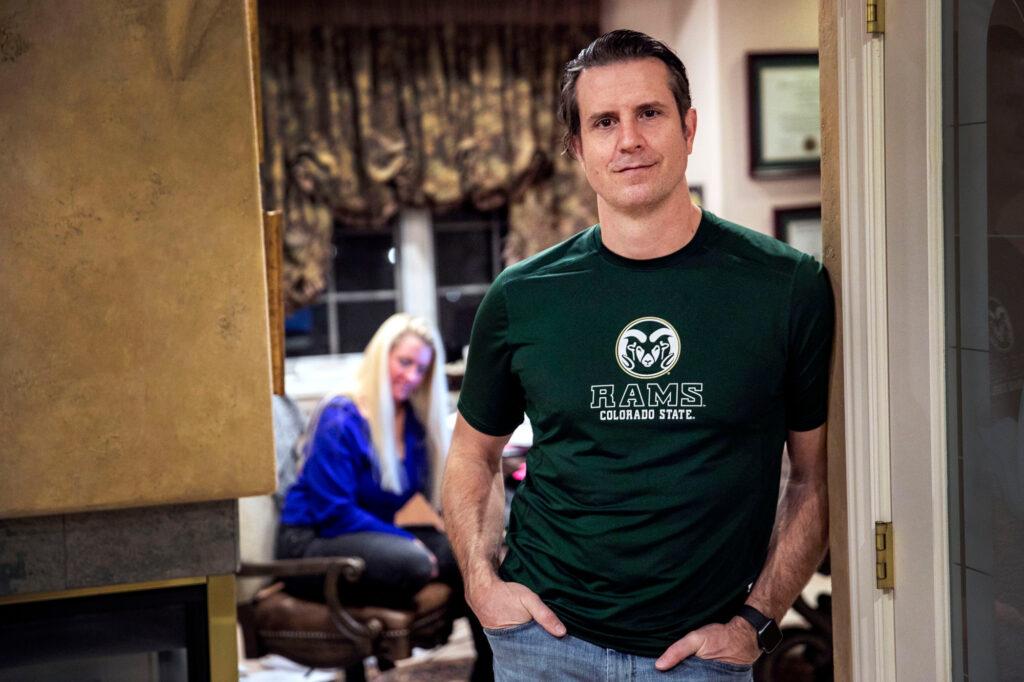
The timing to help is good too with most frontline providers now having been vaccinated, and patient counts down in Colorado hospitals.
“The biggest reason I wanted to volunteer in California is because they need our help and we've been fortunate enough to keep rather good control of (the virus in Colorado),” he said. “Nevertheless, it does help that I have been vaccinated.”
But he warns “we're not over this yet. And Southern California is a cautionary tale of what could happen here in Colorado.”
That’s if its residents don't respect the virus, by keeping up with the public health precautions that have so far allowed it to avoid the biggest COVID-19 waves that have swamped other states.
The proportion of U.S. hospitals nearing a breaking point has doubled since November, according to an analysis of federal hospital data by the Associated Press. More than two in five Americans now live in locations running out of ICU capacity, with just 15 percent of beds still available.
Colorado avoided a post-holiday surge. California did not
An estimated one in three residents in Los Angeles has been infected with the virus. The region’s wave of cases coincides with a new variant, different from the more infectious strains first found in the U.K. and South Africa, called CAL.20C. It’s become one of the main strains in LA County. Thanks to the flood of new cases, hospitals there have faced shortages of staff, even oxygen.
Colorado’s hospitals were headed in that direction too in early December, when hospitalizations and deaths peaked at record levels for the state. But since then key COVID-19 metrics (hospitalizations, cases, positivity, deaths) have trended downward steadily, following renewed implementation of since-eased restrictions in November.
It also appears residents heeded calls to avoid travel and crowded indoor spaces and to wear masks helping Colorado avoid the kind of post-holiday surge of cases seen elsewhere. That improving hospital situation opened the door for some of its providers to give desperately needed help in other states.
The volunteer providers are a bit like reserve soldiers in a war.
“Just having extra bodies, extra hands there to assist, helps to offload some of the pressure on the current staff at a hospital. And then it also gives people a time to rest,” said Dr. Monique Butler, Division Chief Medical Officer with HCA in Tallahassee, Fla. “It's teamwork, it's empathy, right? It's individuals who understand and know how devastating this pandemic has been.”
“It’s all hands on deck (during the pandemic),” said Butler, who until the end of 2020 was the chief medical officer with Swedish Medical Center in Englewood.
At Swedish, a number of nurses, techs and respiratory therapists offered to help on two occasions when things got bad in Texas. That included in El Paso, one of the nation’s hot spots last fall.
The volunteer providers are “already heroic,” said Butler, who noted the logistical challenges, for both hospitals and providers, of juggling duties and mapping out new and changing roles. “They become even more heroic because they put their hands in the air to say, ‘I want to help my fellow colleague, and I want to help the communities.’ Which is amazing.”
Colorado health care workers have volunteered in many other states, and even virtually
It’s not the first time Colorado’s frontline providers have stepped up to help during the pandemic. Some from other systems, like Banner, HealthONE, Centura and SCL Health, have sent employees to states like Arizona, New York, New Jersey and Montana.
A spokeswoman for the state’s hospital association said she’s not aware of other states sending staff to Colorado to help during the fall surge, probably because the whole country was basically experiencing a surge at that time.
The Kaiser physicians sent to California have expertise in critical care pulmonology, anesthesiology, and hospital medicine. Some are assisting with care virtually, including in ICUs and with a virtual ambulatory clinic.
Shifts can be up to 10 days, with providers working in the various hospitals owned and operated by Kaiser Permanente in Southern California. (Unlike in California, KP in Colorado doesn’t own and operate its own hospitals.)
Other Kaiser Permanente regions are pitching in too, including the system’s Hawaii and Mid-Atlantic regions.
As nurse Sara Kollman’s time in LA was winding down, she started to see glimmers of hope with COVID-19 trends showing signs of getting better.
“(It's) heartwarming to actually see open beds and patients being admitted to the hospital that were not COVID-related," she said.
"And the staff, you could just see the relief in their eyes,” as the ratio of providers to patients appeared to be improving.
“Still not completely back to normal, but more normal.”









